Wednesday 7 May 2025
A mother from Macclesfield in Cheshire, who was diagnosed with cancer two years ago is now in complete remission, with no sign of cancer, thanks to a cutting-edge new experimental drug.
Michelle Gidion, 56, is receiving the treatment, as part of a clinical trial, at The Christie NHS Foundation Trust in Manchester for an aggressive type of blood cancer called AML (Acute Myeloid Leukaemia) which is a cancer of the blood and bone marrow.
In February 2023 Michelle had been experiencing bruising and tiredness, and mentioned this to a friend, Pamela, who insisted she went the GP where they took a sample of her blood for testing.
“Pamela saved my life by making me go and get checked out. I put the bruising down to having a very active lifestyle, but now I realise it wasn’t normal. Running a home with four boys was always hectic so I didn’t think being tired was unusual.”
Michelle, and her husband Simon, who have been married for eight years, have a shared love of cars and are Formula One fans – so much so they have named their four sons after famous racing drivers – Ayrton (21), Jenson (20), Rubens (18) and Mika (16).

The family were due to go on a holiday of a lifetime in the May to the French Alps, their first holiday together for four years. It was at the airport, while waiting for the flight, that Michelle received a phone call from a haematologist who broke the news that the blood test results revealed she had leukaemia. The consultant advised her not to board the plane as the platelets in her blood were so low she could potentially bleed to death if she had an accidental injury. The whole family were in shock and had very little time to decide what to do. Not wanting to ruin the long-anticipated dream trip, they chose to fly despite the risk.
“I didn’t know anyone who had had leukaemia and had no idea how dangerous it was to travel.” Michelle said. “I’d been walking up hills only days before and wasn’t feeling unwell. I didn’t want to spoil things for my sons, but as it turned out it was the wrong call to make.”
The situation was so stressful that Michelle became ill as soon as they arrived in France and the family returned home 24 hours later.
Michelle was taken directly to her local A&E from the plane where she spent 48 hours before transferred straight to The Christie where she stayed for five days and had a bone biopsy which confirmed she had AML. She went straight onto a course of chemotherapy which she responded well to and went into remission, but after only five months the cancer returned.
It was suggested Michelle had a stem cell transplant to cure her of cancer, and luckily a perfect match was found with a stem cell donor from the international register. She had the transplant in March 2024 but unfortunately had a reaction and went through a tough five-week-long stay at The Christie. At one point she had to leave her isolation room and be taken to Manchester Eye Hospital to have laser eye surgery on her right eye to correct her vision that had been affected by the treatment.
Despite going through the gruelling transplant procedure and being given an 80% chance of it being successful due to her age and level of fitness, biopsy results in May 2024 led to the devasting discovery that the procedure hadn’t worked.
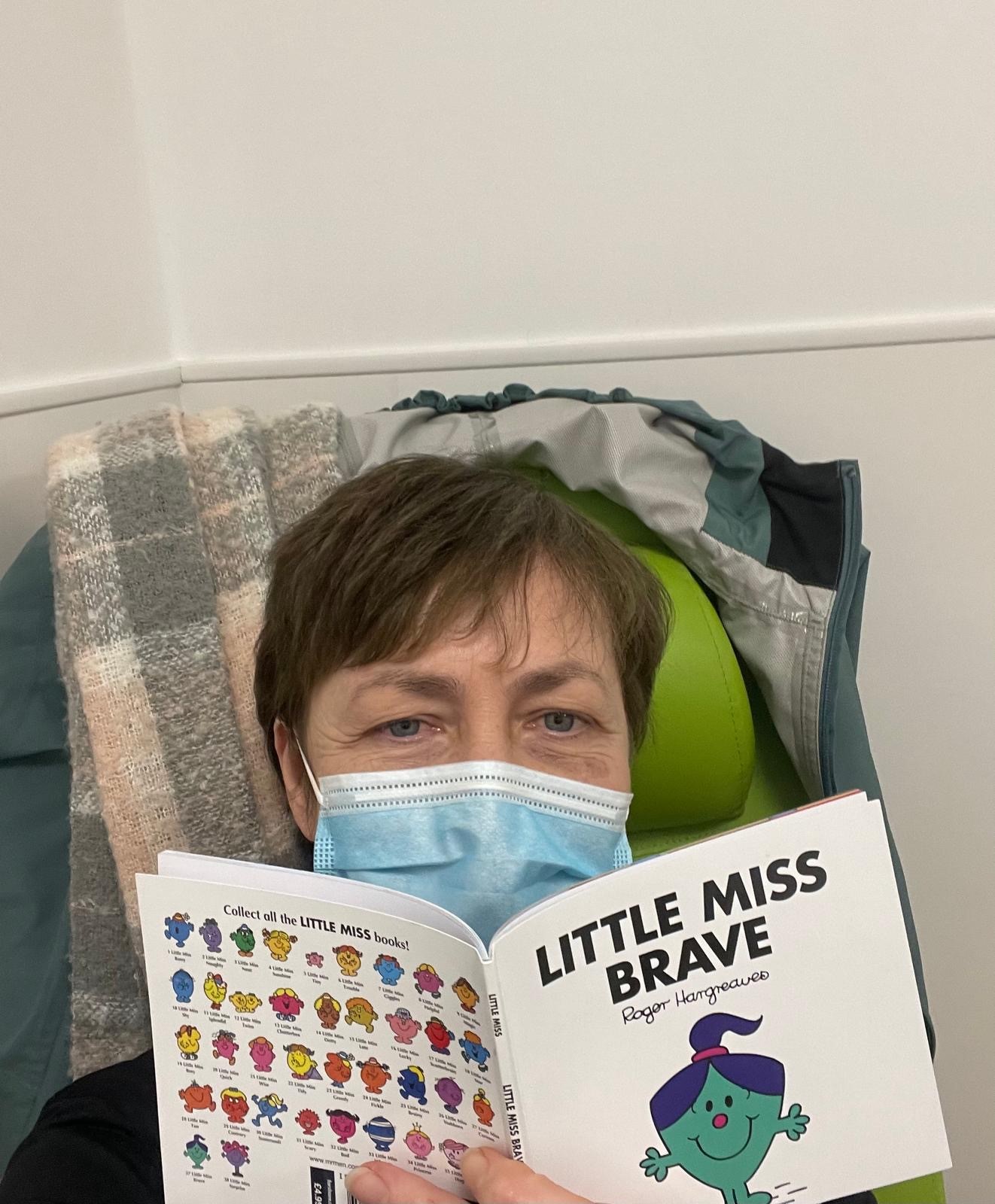
By this point Michelle was frail, with no energy and could barely walk. So in July 2024, with options running out, she was offered the chance to participate in research at the National Institute for Health and Care Research (NIHR) Manchester Clinical Research Facility (CRF) at The Christie NHS Foundation Trust (The Christie) in Manchester. Michelle signed up to an international clinical trial funded by Johnson & Johnson called CAMELOT-1. It is an early phase study for a new type of targeted cancer drug called bleximenib which is a menin inhibitor. Scientists have found that a protein called menin plays a key role in helping leukaemia cells survive and grow in certain types of leukaemia. Menin inhibitors are drugs that block this protein, making it harder for the leukaemia cells to keep multiplying. Without menin’s support, these cancerous cells become weaker and eventually die, allowing the body to start making healthy blood cells again. Michelle takes two tablets of the trial drug every morning and two in the evening and comes to The Christie every four weeks for monitoring.
In November last year (2024), and again in February this year (2025), Michelle had a DLI (donor lymphocyte infusion) from the same stem cell donor to help boost her new immune system from the bone marrow transplant, and last month she was told that the drug has got her into complete molecular remission which means there are currently no detectable signs of cancer in her blood or bone marrow.
Talking about her experience of being on the trial, Michelle Gidion said:
“I’ve been super active all my life. I was a fitness freak in my 20s and I was regularly walking near our home in the foothills of the Pennines on the edge of the Peak District. We are just a very outdoorsy family, so this diagnosis really turned our lives upside down. The trial feels like there’s light at the end of a very long dark tunnel. The drug, together with the DLIs, has got me to a place where I feel a lot better and gradually I’m getting my energy levels back.
“Research is so important. When offered the trial there was no way I wasn’t going to say yes to it. I just want to be alive, so I grabbed it with both hands. It’s the only thing that’s given us hope in the last two years. My four sons have all signed up for the stem cell register now, so hopefully they can help someone in the future and Jenson has recently raised money for blood cancer research. The whole experience has been life changing for our family.”
Dr Emma Searle, Consultant Haematologist who leads the trial at The Christie, and is in charge of Michelle’s care, said:
“With early phase trials where the drug has never been tested on patients before, we are looking at how well participants tolerate the treatment and what dose is safe. We are finding some side effects, which are usually manageable, but most importantly 41% of patients have so far responded which is very promising.”
“We are very pleased with Michelle’s progress on the trial. She has tolerated the drug well with minimal side effects, feels well and can enjoy life. This could potentially be a new therapy for patients with AML who have specific gene mutations and have relapsed after initial treatment, or may in the future be added to standard treatment for newly diagnosed patients to improve outcomes.”
The CAMELOT-1 study is open for recruitment with an aim to recruit 150 participants worldwide.
According to Cancer Research UK data, there are nearly 3,000 new cases of AML in UK every year (which is less than 1% of all new cancer cases) and more than 2,500 AML deaths in the UK every year.
Dr Emma Searle is part-funded by The Christie Charity. Research such as this is central to The Christie Charity’s commitment to supporting The Christie hospital’s vision of ‘learning from every patient’ and trebling the number of patients participating in research by 2030. Studies have shown that cancer patients treated at research-intensive hospitals have better outcomes than those treated in hospitals with little or no research activity. The Charity has pledged to support and fund this goal with £30m over the next five years with the ultimate aim of bringing tomorrow’s treatments to patients faster.
